Vaginal Atrophy
Every part of the body undergoes changes with aging. The most evident and visible change is the skin. Women show great interest in pampering the skin to retain a youthful look. There are several genital changes that are common with aging. Most women are unaware of the genital change particularly after menopause. Reluctance, embarrassment, cultural taboo, ignorance, anxiety, fear - there are many reasons that hold back women from openly discussing about this 'private thing'. Millions of women suffer in silence! Ignorance can mess up not just the physical well-being but emotional well-being as well.
Aging and Vaginal Atrophy - the link
Aging brings a shift in hormone levels. At its peak in teens, it tapers off in thirties. Of the three hormones, estrogen, progesterone and testosterone, vaginal atrophy is directly linked with decline in estrogen levels.
How ?
The role of Estrogen:
1. Stimulate growth of breast tissue.
2. Maintain vaginal blood flow and lubrication.
3. Cause lining of the uterus to thicken during the menstrual cycle.
4. Keep vaginal lining elastic and
5. Perform other functions, including preserving bone.
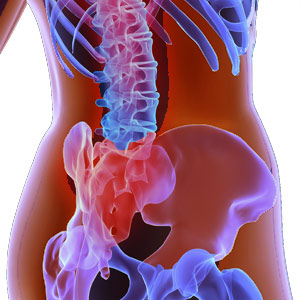
It is clear that the decline in estrogen has a direct impact on the health, structure and functioning of vagina. Prior to menopause, the vaginal lining appears plump, bright red, and moist. The decline leads to thinning, drying and inflammation of the vaginal walls. This is Vaginal Atrophy, a physical condition and not to be understood as an illness.
Though vaginal atrophy is linked to menopause and is ranked as the leading cause of decreased levels of estrogen, it can also happen at any other time when the estrogen levels decline in a woman's body. The possibility is high in smokers, pre-menopausal women who take anti-estrogenic medications or who have medical or surgical conditions that result in decreased levels of estrogen.
- Childbirth and Breastfeeding
- Surgical removal of ovaries
- Cysts on and in the ovaries
- Decreased functioning of the pituitary gland
- Taking certain fertility drugs
- Premature menopause
- Radiation treatment to the pelvic area or chemotherapy
- Medications used to treat cancer, endometriosis, fibroids or infertility (to decrease estrogen levels)
- Stress, depression, rigorous exercise (particularly in young women).
Impact of vaginal atrophy
A survey on the subject shows that vaginal atrophy is widely prevalent amongst postmenopausal women, particularly in United States as compared to other countries.
- Affects overall sexual functioning
- Excessive vaginal discharge
- Itching in the vaginal area
- Painful intercourse
- Loss of libido or diminished sexual desire
- Bleeding after sex
- Discontinuation of sexual activity
- Problems related to sexual arousal or orgasm
- Urinary function problems
- Emotional distress/impacts self-esteem
- Negative consequences on marriage/relationship
- Sleep disturbance/interference with sleep
- Mood changes.
A woman unable to comprehend and correlate to vaginal atrophy may not seek medical attention at all. A simple issue can aggravate into a complex problem. Knowing symptoms and identifying presence of vaginal atrophy prepares a woman to seek medical attention and provides her the much needed care and assurance for a healthy life ahead.
Vaginal atrophy
After menopause most women experience discomfort and uneasiness in the vagina. It is mainly due to falling levels of estrogen which plays an essential role in maintaining the elasticity and health of the genital tissues. This can result in thinning of the tissues around the vagina and reduction in the number of glands that make vaginal mucus. The vaginal mucus becomes thinner, drier, less elastic and more fragile. Some fat issue around the genital area may also reduce. These changes in turn alter the appearance of the area.
Vaginal atrophy or Atrophic vaginitis is the medical term for the condition when these changes produce troublesome symptoms.
Vaginal atrophy symptoms and signs
Vaginal atrophy symptoms often occur within 12 months of the cessation of natural or surgical menstruation or even after couple of years. Most women experience one or several of these vaginal atrophy symptoms. Mild to severe, the degree may also vary. Only 25% of symptomatic women seek medical attention for vaginal atrophy. Knowing symptoms is precursor to seeking medical attention and treatment. If left untreated, vaginal atrophy can result in years of discomfort, with a significant impact on quality of life.
Symptoms (experienced by a woman)
- Decrease in vaginal lubrication
- Vaginal dryness
- Pain during sexual activity
- Discomfort or irritation when wearing tight-fitting clothes
- Tightening of the vaginal wall
- Inability to engage in certain activities
- Increase in urinary tract infections.
Signs (physical manifestation of the condition)
- Change in appearance of the labia and vagina
- Reduced pubic hair
- Lack of vaginal fold.
In addition to these, women may experience other symptoms of menopausal transition like hot flashes, night sweats, mood changes, fatigue, urinary tract infections, urinary incontinence, acne, memory problems etc.
Diagnosing vaginal atrophy
A critical first step towards diagnosis and opting for an effective treatment is to make up your mind and seek medical attention. A woman who suspects to having vaginal atrophy should seek an appointment with her gynecologist or health care provider.
The meeting will primarily aim at recording the personal history of the woman and to check contributing factors that can worsen the symptoms. A pelvic examination is likely to be followed by a visual examination of the external genitalia, vagina and cervix. The purpose is to check any abnormality in the area that helps in making an accurate diagnosis.
After menopause women are prone to urinary infections mainly due to less mucus in the vaginal area. To rule out urinary infections, urine test will be done. An acid balance test to confirm estrogen deprivation is required. If the vaginal pH testing exceeds pH 5.0, it is an indication of estrogen deprivation.
Based on the test report and assessment, a course of treatment will be recommended. Prior to the meeting, prepare for the appointment by engaging in a short exercise. Sometimes during the discussion key points are likely to be missed out.
- List out the signs and symptoms being experienced (the duration and any other specification can also be noted down)
- Write down the medications being taken along with reasons. Include vitamins and supplements as well.
- Prepare a list of questions or doubts to be clarified.
- Prepare the mind to discuss openly including your sex life.
- Examine if counseling with partner will benefit.
Vaginal atrophy treatment
Irrespective of the treatment procedure, be informed that it takes time, weeks or even months to achieve full benefits of effective treatment. After discussing the risks and benefits of the choice of treatment, a persistent approach to seek relief has proved to be rewarding.
Vaginal atrophy treatment option is linked to the magnitude of symptoms, mild, persistent or severe, as the case may be. Each of these options provides relief from specific symptoms. While assessing the risks and benefits of each of these, check with the healthcare provider if the use of condoms or a diaphragm will in any way interfere or impact the choice of a specific treatment option. Most of it is based on personal preference.
Non-hormonal therapies: OTC or over-the-counter lubricants or moisturizing products, moisturizers, water-soluble lubricants provide relief from mild vaginal atrophy symptoms. For best results, the lubricant can be used by both the partners while engaging in sexual activity.
OTC applications: By using non-prescription or OTC lubricants or moisturizers, the sense of discomfort and friction is considerably eased as the application restores moisture in the vaginal area. Available in all drug stores, these can be in the form of gel, liquids and suppositories.
Lubricants: Water, silicone or oil-based, lubricants will not get absorbed by the skin and have to be washed off. The only disadvantage of using an oil-based lubricant is that it can interfere with latex condoms, if used. An unplanned pregnancy can materialize as the oil-based lubricant can break off the condoms.
Moisturizers: Unlike lubricants, moisturizers are absorbed by the vaginal lining to keep the area moisturized. Women can apply moisturizer every few days to avoid vaginal dryness.
Natural oils: Natural oils like vitamin E, coconut oil, olive oil, grape seed oil, sunflower oil are safe natural oils that regularly help hydrate the vulvar skin, strengthen it and even heal the fissures. The oil can be used during or after bathing and even during sexual intercourse.
Vaginal estrogen therapy: If the problems persist or worsen, healthcare providers recommend safe and effective vaginal estrogen therapy for moderate to severe vaginal atrophy symptoms. This is a long-term treatment plan. There are options for consideration. Taking into account specific patient information, the health care provider can help in choosing the most appropriate one.
Vaginal ring: Being a low-dose vaginal estrogen therapy, doctors recommend vaginal ring to even women with a history of cancer, ovary cancer or endometrial cancer.
After inserting the ring into the upper part of the vagina, estrogen is delivered or slowly released from a small, flexible ring. Estrogens released are absorbed into the blood stream through the vaginal walls. The ring remains inserted in the vagina for three months at a time. After three months, a new ring will be replaced. The ring has does not interfere with normal sexual intercourse and there isn't the slightest possibility of the partner knowing it unless the woman decides to share the information.
Use of vaginal ring is contraindicated in women, who are pregnant or breastfeeding, have a medical history of abnormal blood clots, diagnosed with cancer or have vaginal bleeding of an unknown cause.
Prescription estrogen creams: Like the OTC creams, gels and lubricants, prescription estrogen creams help alleviate the dryness and painful intercourse. An applicator is used to insert the cream in low dose into the vagina. The dose is recommended by the healthcare provider after ascertaining the individual needs of each patient. But topical estrogen cannot be used in women with breast cancer.
Prescription estrogen vaginal tablets: Vaginal tablets are placed in the vagina with an applicator twice per week. The duration may change depending on other associated conditions.
Osphena: Approved by the FDA in 2013, Osphena is an oral tablet recommended for women experiencing moderate to severe vaginal atrophy symptoms, especially to relieve painful intercourse. The drug has specific contraindications and hence should not be taken without the recommendation of a health care provider.
Lifestyle changes: Women can follow a combination therapy by bringing modifications in lifestyle.
Ample studies have proved that increase in coital activity is advantageous as it leads to enhanced blood flow to the vagina and keeps the vaginal tissues healthy. Regular sexual intercourse can keep the vaginal tissues healthy, moist, and flexible. If pain during sex is a deterrent, engaging in sexual arousal activities and using a personal lubricant can be helpful.
Also, quitting smoking and consumption of cranberry juice (for urinary tract infections) are effective in relieving symptoms of vaginal atrophy.
Switch over to non-irritating, non-drying soap. Choose a nightgown or long tee-shirt that allows air to circulate around the vagina. Abstain from alcohol, caffeine and antihistamines as these can dry the mucous membranes.
Look at exercise as a means to strengthen the muscles around the area. Kegels exercises have proved to be beneficial. The exercise involves tightening and releasing the muscles around the vagina and anus several times. If done on a daily basis, the exercise helps in strengthening the pelvic floor muscles, improves sexual satisfaction and is effective in providing relief from urinary incontinence.
There are specific Yogic postures that are effective in dealing with anxiety, stress, and fatigue and strengthen the pelvic muscle as well. All pelvic floor exercises tone the vaginal tissues. Choose exercises and try these poses. Note down that which brings most relief and practice these poses on a regular basis. Integrate these Yogic postures with the regular exercise regimen.
Prevention is better than cure
Complete prevention may not be realistic but a self-care program can reduce the chances of developing vaginal atrophy and considerably reduce the discomfort.
- Pelvic floor exercises are help strengthen the pelvic floor muscles. Better sexual function, bladder and bowel control, great benefits can be derived.
- Eat a balanced diet to provide the vital nutrients and vitamins for the healthy functioning of the body.
- Drink plenty of water to remain hydrated.
- If contraceptives are causing vaginal dryness consider changing the brand.
- Avoid scented perfumes, shaving, waxing in the genital area as it may aggravate the discomfort.
- Use plain water to wash the genital area and maintain hygiene.
- Avoid tight-fitting clothes to allow considerable air movement and to avoid friction while walking etc.
- Prefer cotton underwear and change them every time after a shower.
Top of the Page: Vaginal Atrophy
Tags:#vaginal atrophy

Enlarged Uterus
Bacterial Vaginosis
Yeast Infection
Irregular Menstrual Cycle
PMS - Menstruation
Dysmenorrhea
Hypomenorrhea
Mid Cycle Bleeding
Pelvic Organ Prolapse
Vaginal Atrophy
Cervix Cancer
Abnormal Pap Smear
Polycystic Ovarian Syndrome
Ovulation Pain
Uterine Prolapse
Fibroid Tumor
Menorrhagia
Endometriosis Symptom
Galactorrhea
Hysterectomy
Blocked Fallopian Tubes
Menopause and Weight Gain
Premature Menopause
Surgical Menopause
Other health topics in TargetWoman Women Health section:
General Women Health

Women Health Tips - Women Health - key to understanding your health ...
Cardiac Care
Women's Heart Attack Symptoms - Identify heart problems...
Skin Diseases
Stress Hives - Red itchy spots ...
Women Disorders
Endocrine Disorder - Play a key role in overall wellbeing ...
Women's Reproductive Health
Testosterone Cream for Women - Hormone replacement option ...
Pregnancy
Pregnancy - Regulate your lifestyle to accommodate the needs of pregnancy ...
Head and Face
Sinus Infection - Nearly 1 of every 7 Americans suffer from ....
Women and Bone Care
Slipped Disc - Prevent injury, reduce pain ...
Menstrual Disorders
Enlarged Uterus - Uterus larger than normal size ...
Female Urinary Problems
Bladder Problems in Women - Treatable and curable ...
Gastrointestinal Disorders
Causes of Stomach Ulcers - Burning feeling in the gut ...
Respiratory Disorders
Lung function Test - How well do you breathe ...
Sleep Management

Insomnia and Weight Gain - Sleep it off ...
Psychological Disorders in Women
Mood swings and women - Not going crazy ...
Supplements for Women
Women's Vitamins - Wellness needs...
Natural Remedies

Natural Diuretic - Flush out toxins ...
Alternative Therapy
Acupuncture Point - Feel the pins and needles ...
Top of the Page: Vaginal Atrophy
Popularity Index: 101,310

