Dysmenorrhea

Dysmenorrhea or dysmenorrhea is the syndrome of painful menstruation and as such is not life threatening. But dysmenorrhea can be debilitating and psychologically taxing for many women. It can wreak havoc in the day to day life of a woman causing physical strain coupled with emotional distress. Dysmenorrhea is mostly noticed in late teens and twenties and gradually declines with age.
Some women may experience increased menstrual pain in their late thirties and forties as their endocrine systems prepare for menopause by decreasing hormone levels and low fertility. Dysmenorrhea is usually less severe after a woman has had a baby. Read on to learn more about the causes of dysmenorrhea. Understand the various treatments for dysmenorrhea.
What is dysmenorrhea?
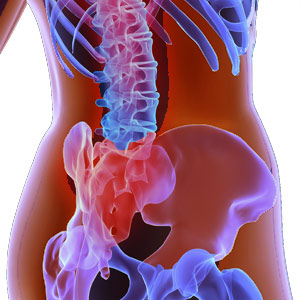
Menstrual cramps are caused by strong contractions in the uterus. During a contraction, it sometimes can press against the nearby blood vessels thereby cutting off supply of oxygen to the muscle tissues. Pain results when part of the muscle loses supply of oxygen for a brief period. Dysmenorrhea involves painful cramps during menstrual periods that are accompanied by sharp intermittent pain or dull throbbing pain usually in the pelvis or lower abdomen.
The pain may precede menstruation by several days or may accompany it. The pain usually subsides as menstruation tapers off. While in some women the pain is severe enough to prevent normal daily function, for others the discomfort would simply be annoying. It is also observed that dysmenorrhea is responsible for significant absence from work or school.
Dysmenorrhea signs and symptoms
- Cramping of the muscle tissues in the uterus
- Sharp pains in the lower abdomen, lower back and thighs.
- Nausea and vomiting
- Headache and dizziness
- Diarrhea occasionally
- Lack of energy
- Frequency in urination
- Depression, nervousness and irritability
- Infertility symptoms
Types of dysmenorrhea
Primary dysmenorrhea: Primary dysmenorrhea involves no physical abnormality. It usually begins six to twelve months after menarche once the regular ovulatory cycle has been established. It tends to be a lifelong condition.
Secondary dysmenorrhea: This condition involves an underlying physical cause. The onset of secondary dysmenorrhea is usually during the thirties and later. This could involve endometriosis or uterine fibroids or pelvic inflammatory diseases.
Diagnosis of dysmenorrhea
Diagnosis of dysmenorrhea is made certain after the physician rules out other menstrual disorders, medical conditions or medications that may be causing the condition. Pelvic ultrasonography is considered in women who are suspected to have secondary dysmenorrhea. Other imaging modalities are also warranted if suspicion of secondary dysmenorrhea is high. A laparoscopy or hysteroscopy may be considered for further investigations.
Causes of dysmenorrhea
During menstruation, some pain is common. But excessive pain is not. Dysmenorrhea usually coexists with heavy blood loss. Prominent causes of primary dysmenorrhea are
- Early age at menarche, say less than twelve years of age.
- Nulliparity
- Smoking
- Family history of primary dysmenorrhea
- Heavy and prolonged menstrual flow
- Obesity
Causes of secondary dysmenorrhea
- Endometriosis occurs especially if dysmenorrhea begins after age twenty.
- Strong and prolonged contractions of the muscular wall of the uterus cause pain. These may be due to concentration of prostaglandins which are hormones found in the cervix and uterus. Research studies reveal that women with dysmenorrhea produce and excrete more prostaglandins than those who do not suffer any such discomfort.
- Adenomyosis - where the tissue that lines the uterus begins to grow within the muscular walls of the uterus.
- Pelvic inflammatory disease caused by sexually transmitted bacteria.
- Sometimes use of intrauterine devices can cause dysmenorrhea.
- Non cancerous uterine fibroids and uterine polyps that protrude from the lining of the uterus can cause secondary dysmenorrhea.
- Leimyomata or fibroids, ovarian cysts and endometrial carcinoma can also contribute to dysmenorrhea.
Use of caffeine or nicotine can worsen dysmenorrhea. It is often found that the degree of dysmenorrhea varies according to the general health and mental state. Certain emotional and psychological factors although cannot cause pain, can worsen the pain or cause some women to be less responsive to treatment. Dysmenorrhea can be found in people with family history of such a condition. Lack of exercise and poor diet can also increase the risk of dysmenorrhea.
Treatment for dysmenorrhea
Specific treatment for dysmenorrhea is determined by the physician based on certain parameters like:
- Age of the patient, overall health and medical history
- Extent of the condition
- Primary or secondary cause of dysmenorrhea
- The tolerance of patients to specific medications, procedures and therapies
- The opinion or preference of the patient.
Usually NSAIDs (Nonsteroidal anti inflammatory drugs) such as ibuprofen and naproxen are very effective in the treatment of primary dysmenorrhea. Oral contraceptives are 90% effective in improving primary dysmenorrhea. They work by reducing the menstrual blood volume and suppressing ovulation. The production of prostaglandins is reduced thereby reducing the severity of the cramps. It may take up to three months for the oral contraceptive to be effective.
Myomectomy, polypectomy or dilation and curettage may be needed in some cases of secondary dysmenorrhea. Endometriosis is treated with several medical options including hormonal contraception like gonadotropin releasing hormone Gn-RH which stops ovary functions and progestational agents. Using heat pads or hot water bottle across the abdomen or back, hot bath or shower may help. Abdominal massages, vitamin supplements and dietary modifications can give some relief from the pain.
Top of the Page: Dysmenorrhea
Tags:#dysmenorrhea #causes of dysmenorrhea #treatment of dysmenorrhea

Enlarged Uterus
Bacterial Vaginosis
Yeast Infection
Irregular Menstrual Cycle
PMS - Menstruation
Dysmenorrhea
Hypomenorrhea
Mid Cycle Bleeding
Pelvic Organ Prolapse
Vaginal Atrophy
Cervix Cancer
Abnormal Pap Smear
Polycystic Ovarian Syndrome
Ovulation Pain
Uterine Prolapse
Fibroid Tumor
Menorrhagia
Endometriosis Symptom
Galactorrhea
Hysterectomy
Blocked Fallopian Tubes
Menopause and Weight Gain
Premature Menopause
Surgical Menopause
Other health topics in TargetWoman Women Health section:
General Women Health

Women Health Tips - Women Health - key to understanding your health ...
Cardiac Care
Women's Heart Attack Symptoms - Identify heart problems...
Skin Diseases
Stress Hives - Red itchy spots ...
Women Disorders
Endocrine Disorder - Play a key role in overall wellbeing ...
Women's Reproductive Health
Testosterone Cream for Women - Hormone replacement option ...
Pregnancy
Pregnancy - Regulate your lifestyle to accommodate the needs of pregnancy ...
Head and Face
Sinus Infection - Nearly 1 of every 7 Americans suffer from ....
Women and Bone Care
Slipped Disc - Prevent injury, reduce pain ...
Menstrual Disorders
Enlarged Uterus - Uterus larger than normal size ...
Female Urinary Problems
Bladder Problems in Women - Treatable and curable ...
Gastrointestinal Disorders
Causes of Stomach Ulcers - Burning feeling in the gut ...
Respiratory Disorders
Lung function Test - How well do you breathe ...
Sleep Management

Insomnia and Weight Gain - Sleep it off ...
Psychological Disorders in Women
Mood swings and women - Not going crazy ...
Supplements for Women
Women's Vitamins - Wellness needs...
Natural Remedies

Natural Diuretic - Flush out toxins ...
Alternative Therapy
Acupuncture Point - Feel the pins and needles ...
Top of the Page: Dysmenorrhea
Popularity Index: 100,783

